By Robert Gorter, MD, PhD, et. al.
Robert Gorter, MD, PhD, is emeritus professor of the University of California San Francisco (UCSF)
Since Dr. Robert Gorter opened his own clinic in Amsterdam in 1973, he was always worried and hesitant to order X-rays and CT Scans as they became available during the 1970’s. All personnel of the radiology department left the patient alone and where hiding behind massive lead doors during the procedure. And radiologists are never to be seen when patients are being exposed: only their MTA’s…
Dr. Gorter studied a lot the literature over the last 15 years, and to the best of his knowledge, one can summarize the current peer-reviewed literature as follows:
- Modern Western (academic) medicine would never have never been this far without imaging devices like X-rays and scans. There are clear benefits of making X-rays, CT & PET scans, etc. But, each time a patient undergoes exposure to radiation of any kind, the necessity, the risks and benefits should be carefully considered in each patient and one should be careful with “protocols” as: “this is how we do it; these are our standards.”
- Routine scans “to have a look” should be prevented. There are several very good surrogate markers other than scans to follow, for instance, a cancer patient over time.
- Children need extra attention and probably by radiologists, specialized in pediatric applications.
- All studies mention the financial interests by doctors and institutions, and in the USA, the “ready-to-sue” culture to order more scans than necessary.
- The bottom line is that if a patient undergoes four CT scans per year, the risk to develop a second primary tumor is 2%; and more than four the chances increases exponentially.
The surprising dangers of CT scans and X-rays
Patients are often exposed to cancer-causing radiation for little medical reason, a Consumer Reports investigation finds
When James Duncan, M.D., a radiologist at Washington University in St. Louis, experienced intense pain in his abdomen in 2010, he rushed to a local emergency room. His doctors suspected kidney stones, but they wanted to be sure, so they ordered a CT scan. Duncan remained motionless as the machine captured a detailed, 3D image of his abdomen. He knew that the test was done when the machine stopped whirring. So he was surprised when the scanner kicked back on after a few seconds.
“I later learned that the technician running the CT mistakenly believed that the first scan didn’t include the top of my kidneys, and decided to acquire more images ‘just to be sure,’ ” Duncan says. “The irony: I was getting ready to give a lecture on reducing radiation exposure from medical imaging. And there I was, reluctantly agreeing to a CT scan and then getting overexposed.”
Duncan will never know whether that specific scan caused any long-term harm, because it’s almost impossible to link radiation exposure from any one medical test to a future illness. But like other researchers, he knows that doctors today order millions of radiation-based imaging tests each year, that many of them are unnecessary, and that the more radiation people are exposed to, the greater their lifetime risk of cancer, or in case of cancer patients, to develop a second primary malignancy.
X-rays have been used for almost 120 years, but the introduction of computed tomography, or CT scans, in the 1970s, was revolutionary. The new tests, which use multiple X-ray images, allowed doctors to see with unprecedented precision the inner workings of the human body, and earned the inventors of the device the 1979 Nobel Prize in medicine. Use of the tests grew quickly, rising from fewer than 3 million per year in 1980 to more than 80 million now.
But recent research shows that about one-third of those scans serve little if any medical purpose. And even when CT scans or other radiology tests are necessary, doctors and technicians don’t always take steps to limit radiation exposure.
All of that exposure poses serious health threats. Researchers estimate that at least 2 percent of all future cancers in the U.S.—approximately 29,000 cases and 15,000 deaths per year—will stem from CT scans alone. Even some standard X-rays, which expose you too much smaller amounts of radiation, can pose risks if you undergo multiple ones.
“No one says that you should avoid a CT scan or other imaging test if you really need it, and the risk posed by any single scan is very small,” says Marvin M. Lipman, M.D., Consumer Reports’ chief medical adviser. “But the effect of radiation is cumulative, and the more you’re exposed, the greater your cancer risk. So it’s essential that you always ask your doctors why they are ordering an imaging test and whether your problem could be managed without it.”
Question: Given those risks, why are we—and our doctors—so scan-happy?
The number of people estimated to die each year in the USA because of cancers caused by the radiation in CT scans alone is 20.000.
For one thing, patients aren’t necessarily aware of the danger. A new Consumer Reports survey of 1,019 U.S. adults found that people are seldom told by their doctors about the risks of CT scans and other radiology tests. It’s no surprise, then, that only 7 percent of those who had a non-dental X-ray and 2 percent of those who had a CT scan thought they might have received the tests unnecessarily. And only 4 percent ever told their doctor they did not want a CT scan. “That’s worrisome,” says Lipman’s colleague at Consumer Reports, Orly Avitzur, M.D. “Patients need to take the lead on this because their doctor may not.”
Other studies show that doctors themselves often underestimate the dangers CT scans pose. Moreover, some doctors or their hospitals may actually have a financial incentive to order the tests.
“Health care professionals shouldn’t have the right to image children or adults unless they first show that they can do it safely and appropriately, and most of the time in this country, that’s not happening,” says Stephen J. Swensen, M.D., medical director at the Mayo Clinic in Rochester, Minn. “If the scan isn’t necessary or emits the wrong dose of radiation, the risks far outweigh the benefits.”
Risks of Exposure to Radiation
Regular CT scans can expose you to as much radiation as 250 chest X-rays. And then PET-CT scans are not even mentioned here. Their risks are much higher as he two forms of radiation are combined: X-rays and radioactive (nuclear) radiation combined.
CT emits a powerful dose of radiation, in some cases equivalent to about 200 chest X-rays, or the amount most people would be exposed to from natural sources over seven years. That dose can alter the makeup of human tissue and create free radicals, molecules that can wreak havoc on human cells. Your body can often repair that damage—but not always. And when it doesn’t, the damage can lead to cancer.
Cancers from medical radiation can take anywhere from five to 60 years to develop, and risk also depends on age and lifestyle; and the number of CT scans. That’s why scientists struggled in early attempts to quantify the danger of medical radiation. Until recently, researchers often relied on evidence from the atomic bomb attacks on Hiroshima and Nagasaki. But now research shows that today’s medical patients are being harmed, too.
New evidence comes from a 2013 Australian study that looked at more than 680,000 people who had CT scans as children and compared them with some 10 million children who did not have a CT scan. The researchers determined that for every 10,000 young people scanned, 45 would develop cancer over the next 10 years, compared with 39 cancers among 10,000 people not screened. Overall, people scanned had a 24 percent increased cancer risk, and each additional scan boosted risk an additional 16 percent. Children who had one before the age of 5 faced a 35 percent spike in cancer risk, reflecting the fact that young bodies are more vulnerable to radiation.
Other researchers estimate that for every 1,000 children who have an abdominal CT scan, one will develop cancer as a result. And a 2012 study that looked at almost 180,000 British children linked CT scans to higher rates of leukemia and brain cancer.
“All too often children are receiving adult-sized doses of radiation, which is many times the amount they need,” Swensen says. “The dose directly increases the risk of leukemia or a solid tumor. And that’s not regulated today.”
Radiation poses a smaller risk to older people, in part because there is less time for cancer to develop in them, explains David Brenner, Ph.D., director of the Center for Radiological Research at Columbia University. But, he points out adults actually receive far more scans than children do, “so the bigger issue is actually with adults.” Research also suggests that, contrary to expectations, the risk of radiation-induced cancer, notably of the lungs, doesn’t decline as we age.

A standard CT scan apparatus.
One scan leads to another
One of the insidious ways that unnecessary CT scans increase risk is that a single CT test often leads to another, then another. A disturbing example of that dangerous cascade was featured in an article in the September 2014 issue of the Journal of Patient Safety, co-authored by John Santa, M.D., and medical director of the Consumer Reports Health Ratings Center.
An 11-year-old girl received a CT scan because of possible appendicitis. That was the first mistake: An ultrasound, which does not emit radiation, is the best initial test in such situations. The second error occurred when her CT showed a normal appendix but her doctors noted a spot on one lung and decided that it warranted a follow-up CT. Such incidental findings are so common doctors have a name for them: incidentalomas.

CT scans can exposes a patients to as much radiation as 250 – 450 chest X-rays.
Expert advice is to ignore the vast majority of those results because slight abnormalities seen on scans are very common but rarely harmful. Yet many doctors find the urge to order follow-up tests irresistible. For the 11-year-old girl, the CT didn’t reveal a tumor or any other problem, but over the next two years her doctors recommended repeat scans of her lungs, all of which would further increase her cancer risk.
“Stories like this occur every day in the United States,” Santa and his co-authors wrote. “This unfortunate sequence of patient harm, waste, and needless anxiety could have been completely avoided with an ultrasound. None of this had to happen. None of this has to happen.”
Why there’s so much over use?
The main reasons for excessive scanning are:
Financial incentives. Overuse is caused “not just by greed and money, but that’s part of it,” says Swensen of the Mayo Clinic. Most doctors are paid by volume, he notes, so they have an incentive to order lots of tests. And many doctors and clinics have invested in radiology equipment. Such physicians order far more CT scans and other imaging tests, research shows.
Fear of lawsuits. This is typical in the USA as American like to sue for almost anything. Almost 35 percent of imaging tests are ordered mainly as a defense against lawsuits, not because of true medical need, according to a study presented at the 2011 meeting of the American Academy of Orthopedic Surgeons.
Uninformed physicians. In a 2012 study of 67 doctors and medical providers caring for patients undergoing abdominal CT, fewer than half knew that the scans could cause cancer. In another study, only 9 percent of 45 emergency-room physicians said they knew that CT scans increased cancer risk.
Misinformed patients. Fewer than one in six patients in our survey said their doctors had warned them about the radiation risks of medical imaging. It’s not surprising, then, that many patients have mistaken assumptions about the dangers of medical radiation. For example, almost as many people in our survey (17 percent) were very concerned about magnetic resonance imaging (MRI), which doesn’t emit radiation, as were concerned about CT scans (19 percent).
Patient demand. When you or your child is in pain, it’s normal to want an imaging test to find out the cause. But that’s often not necessary or wise. Many back-pain sufferers, for example, ask their doctor for an X-ray or CT scan (and many doctors acquiesce) even though expert guidelines say that such tests are usually warranted only if the pain lasts a month or longer.
Lack of consensus and regulation. About one-third of the people in our survey assumed that laws strictly limit how much radiation a person can be exposed to during a CT scan. In fact, unlike mammography, there are no federal radiation limits for any kind of CT imaging.
There are also no national standards for the training or certification of technologists (professionals who operate the imaging machines). Some states allow almost anyone to work the equipment. The government relies on three outside accrediting organizations—the American College of Radiology, the Intersocietal Accreditation Commission, and The Joint Commission—to ensure the safety of advanced imaging facilities. But each group has different quality and safety standards.
“As you go around the country, you see all this variation in how medical imaging is being used and adherence to best practices,” Duncan says. Starting in 2016, the Centers for Medicare and Medicaid Services (CMS) plans to cut reimbursement rates if CT machines don’t have the most recent safety features. It has been reported that about one-third of the scanners now used across the country won’t meet those new CMS standards.
What should a patient and their beloved ones know and do?
Here is Dr. Gorter and his colleague’s advice on what to do before one gets any radiation-based imaging test:
- Ask why the test is necessary. Of course, don’t turn down a test if it’s really needed. But they’re often not. So ask why the test is being done, how the results will be used, what will happen if you don’t get the test, how much radiation you will be exposed to, and whether there is a radiation-free alternative like MRI or ultrasound that could be substituted. For more, read the report “When to Question CT scans and X-rays.”
- Check credentials. There’s no guarantee that the equipment will work or that the providers are skilled. But there are some indicators. Ask whether the facility is accredited by the American College of Radiology, whether the CT technologists are credentialed by the American Registry of Radiologic Technologists, and whether the person interpreting the scans is a board-certified radiologist or pediatric radiologist. Also check online to see whether the radiology professional, imaging facility, or referring physician has joined efforts to reduce the overuse of medical imaging, such as Image Gently, which focuses on children, and Image Wisely for adults.
- Get the right dose for your size. The smaller or thinner you are, the lower the radiation dose you need. The circumference of your chest, hips, thigh, or waist can also change the dose. So before you get scanned, ask the person taking the test whether they’ve factored all of that into your scan.
- Ask for the lowest effective dose. The strength of the radiation dose used during a CT scan can vary tremendously, even when done in the same institution and for the same medical purpose. Avoiding the highest of those doses could almost cut in half the number of future radiation-related cancers, according to a 2013 study in the journal JAMA Pediatrics.
- Avoid unnecessary repeat scans. The Institute of Medicine reports that $8 billion is spent annually on repeat testing, much of it unnecessary. That often happens because doctors may prefer to get a new test rather than look at a previous one. So let your doctor know if you recently had an imaging test. To track your scans, jot down the date, facility, and ordering physician in a journal. And ask for copies of your scans to be put on a CD so that you can show them to new doctors.
Get a second opinion if you are not sure and there is no emergency procedure necessary. . .
What to do if one’s doctor owns a CT scanner or has a financial interest in an imaging center?
An in-office CT might seem convenient, but it carries an inherent financial conflict of interest. And studies have found that physicians who own scanners or are part owners of radiology clinics use imaging substantially more than others. If one’s doctor owns a scanner, ask why you need the CT or whether another test might be an option. And if he is sending you to a radiology clinic, ask whether he is financially affiliated with it.
What to do if one’s doctor recommends a “whole-body” CT scan
Those scans are often touted as a way to detect early signs of cancer and heart disease. But most scans—and up to 80 percent in older people—have at least one abnormality that shows up on the exam. Almost all of the abnormalities are harmless, yet about one-third of patients are referred to follow-up imaging, according to a 2013 study. And whole-body CT scans expose you to much more radiation than regular CT scans. One study determined that for every 1,250 45-year-old adults who have the exam, one will die of cancer as a result.
What if one’s dentist recommends a 3D dental scan?
The CT technique, called cone-beam CT, exposes children to about six times more radiation than traditional dental X-rays. The American Dental Association says that children rarely need them before orthodontic procedures. And several studies have shown that for any given dose of radiation, children are three to four times more likely than adults to develop malignancies, in part because their cells are more sensitive to radiation.
What are the options?
Ultrasound
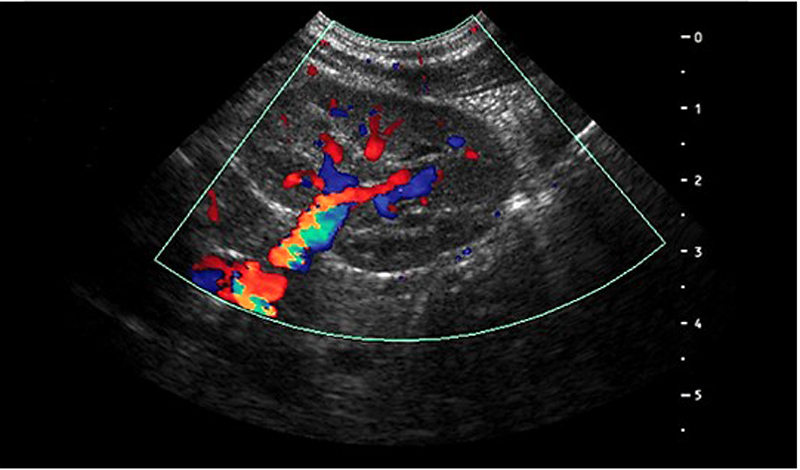
A typical picture obtain by ultrasound (echography, sonography).
High-frequency sound waves sent through the body create echoes as they bounce off organs and tissues. Echoes are then turned into real-time images called sonograms. Produces fairly good images of soft-tissue disease, but they’re not very detailed, especially in obese patients. Radiation exposure: none.
MRI: Magnetic Resonance Imaging
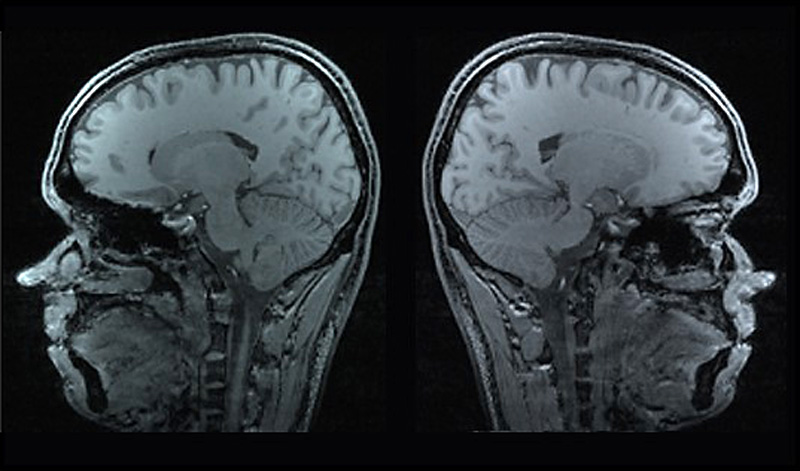
Typical images of an MRI scan of the brain.
Magnetic resonance imaging uses magnets and radio waves to create detailed images that can help spot cancers and soft-tissue problems. Patients are enclosed in the machine for 20 minutes to sometimes 90 minutes before the image is captured. Radiation exposure: none.
IN CASE THERE ARE NO OTHER OPTIONS
CT: Computed Tomography
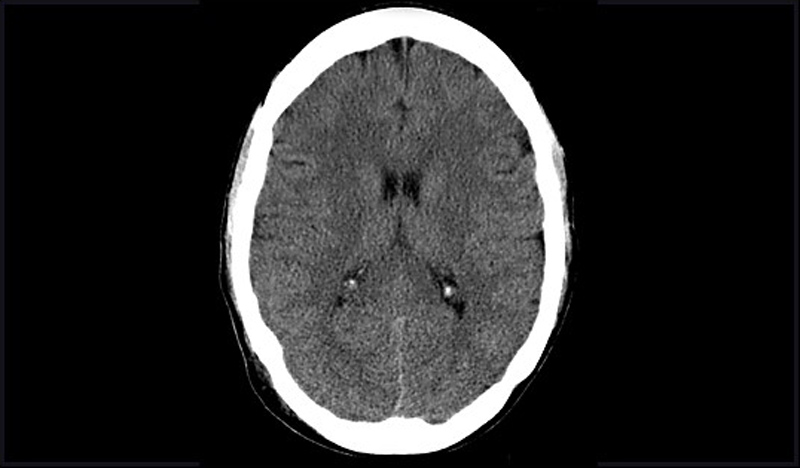
A typical CT image of the brain.
Computed tomography uses a pencil-thin X-ray beam to create a series of images from multiple angles, which are then transferred to a computer, creating a 3D image that can be enlarged and rotated onscreen. Excellent for looking at soft tissue. Radiation exposure: moderate to high.
In total, or whole-body, CT creates pictures of nearly every area of the body—from the chin to below the hips. This procedure, which is used routinely in patients who already have cancer, can also be used in people who do not have any symptoms of disease. However, whole-body CT has not been shown to be an effective screening method for healthy people. Most abnormal findings from this procedure do not indicate a serious health problem, but the tests that must be done to follow up and rule out a problem can be expensive, inconvenient, and uncomfortable. In addition, whole-body CT can expose people to relatively large amounts of ionizing radiation—about 12 mSv, or four times the estimated average annual dose received from natural sources of radiation. Most doctors recommend against whole-body CT for people without any signs or symptoms of disease.
Reminder: Just one CT scan of the abdomen or the pelvis equals about 10 millisieverts, more radiation than most residents of Fukushima, Japan, absorbed after the Fukushima Daiichi nuclear power plant accident in 2011.
PET: Positron Emission Tomography
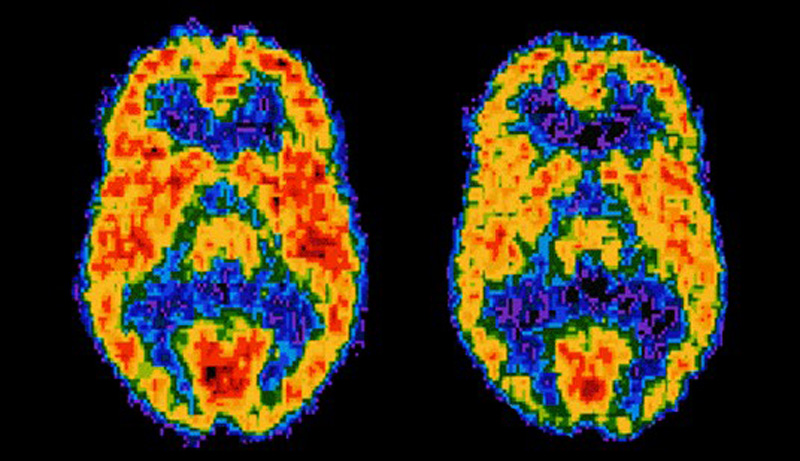
Characteristic image of a PET scan.
Positron emission tomography requires the patient to ingest a radioactive tracer, usually thru injection, that lands in cells, especially cancer cells. Some machines that are used combine PET and CT scans. Radiation exposure: medium to high. The combination of X-radiation and radioactive (nuclear) radiation has never been studied but very likely to be worse than each exposure to each radiation separately. When a patient receives radioactive material to ingest and per infusion the patient gets instructed for the next 3-4 days not to have a child close (like hugging or sitting on one’s lap) to prevent a child from being exposed to radioactive radiation…..
Combined PET-CT uses two imaging methods, CT and positron emission tomography (PET), in one procedure. CT is done first to create anatomic pictures of the organs and structures in the body, and then PET is done to create colored pictures that show chemical or other functional changes in tissues.
Different types of positron-emitting (radioactive) substances can be used in PET. Depending on the substance used, different kinds of chemical or functional changes can be imaged. The most common type of PET procedure uses an imaging agent called FDG (a radioactive form of the sugar glucose), which shows the metabolic activity of tissues. Because cancerous tumors are usually more metabolically active than normal tissues, they appear different from other tissues on a PET scan. Other PET imaging agents can provide information about the level of oxygen in a particular tissue, the formation of new blood vessels, the presence of bone growth, or whether tumor cells are actively dividing and growing.
Combining CT and PET may provide a more complete picture of a tumor’s location and growth or spread than either test alone. The combined procedure may improve the ability to diagnose cancer, to determine how far a tumor has spread, to plan treatment, and to monitor response to treatment. Combined PET-CT may also reduce the number of additional imaging tests and other procedures a patient needs.
How Much Do CT Scans Increase the Risk of Cancer?
A significant number of researchers re-evaluate the safety of radiation used in medical imaging.
Ever since physicians started regularly ordering CT (computed tomography) scans four decades ago, researchers have worried that the medical imaging procedure could increase a patient’s risk of developing cancer. CT scanners bombard the human body with x-ray beams, which can damage DNA and create mutations that spur cells to grow into tumors.
Doctors have always assumed, however, that the benefits outweigh the risks. The x-rays, which rotate around the head, chest or another body part, help to create a three-dimensional image that is much more detailed than pictures from a standard x-ray machine. But a single CT scan subjects the human body to between 150 and 1,100 times the radiation of a conventional x-ray.
A handful of studies published in the past decade have rekindled concerns. Researchers at the National Cancer Institute estimate that 29,000 future cancer cases could be attributed to the 72 million CT scans performed in the country in 2007. That increase is equivalent to about 2 percent of the total 1.7 million cancers diagnosed nationwide every year. A 2009 study of medical centers in the San Francisco Bay Area also calculated an elevated risk: one extra case of cancer for every 400 to 1,000 routine chest CT exams.
The reliability of such predictions depends, of course, on how scientists measure the underlying link between radiation and cancer in the first place. In fact, most estimates of the excess cancer risk from CT scans over the past several decades rely largely on a potentially misleading data set: cancer rates among the long-term survivors of the atomic bomb blasts in World War II.
“There are major concerns with taking the atomic bomb survivor data and trying to understand what the risk might be to people exposed to CT scans,” says David Richardson, an associate professor of epidemiology at the University of North Carolina Gillings School of Global Public Health who has done research on the atomic bomb survivors.
About 25,000 atomic bomb survivors were exposed to relatively low doses of radiation comparable to between one and three CT scans. The number of cancer cases that developed over the rest of their lives is not, however, large enough to provide the necessary statistical power to reliably predict the cancer risk associated with CT scans in the general population today. Given these difficulties, as well as renewed concerns about radiation levels and the lack of mandatory standards for safe CT exposure (in contrast to such procedures as mammography), a dozen groups of investigators around the world have decided to reevaluate the risk of CT radiation based on more complete evidence.
A growing number of clinicians and medical associations are not waiting for definitive results about health risks and have already begun figuring out how to reduce radiation levels. Two radiologists at Massachusetts General Hospital, for example, think that they can decrease the x-ray dosage of at least one common type of CT scan by 75 percent without significantly reducing image quality. Likewise, a few medical associations are trying to limit superfluous imaging and prevent clinicians from using too much radiation when CT scanning is necessary.
For obvious ethical reasons, researchers cannot irradiate people solely to estimate the cancer risk of CT. So scientists turned to data about survivors of the atomic bombs dropped on Hiroshima and Nagasaki in August 1945. Between 150,000 and 200,000 people died during the detonations and in the months following them. Most individuals within one kilometer of the bombings perished from acute radiation poisoning, falling debris or fires that erupted in the immediate aftermath of the attack. Some people within 2.5 kilometers of ground zero lived for years after exposure to varying levels of gamma rays, from a high end of more than three sieverts (Sv)—which can burn skin and cause hair loss—to a low end of five millisieverts (mSv), which is in the middle of the typical range for CT scans today (2 to 10 mSv). A sievert is an international unit for measuring the effects of different kinds of radiation on living tissue: 1 Sv of gamma rays causes the same amount of tissue damage as 1 Sv of x-rays (Storrs, 2013).
CT scan is appropriate when need outweighs risks
Scott D. Stevens, MD, UK radiologist.
Two studies in the UK are important because they raise awareness about exposure to radiation associated with a CT scan. In 66% of all hospitals in the UK expose patients up to 11 times (!) more X-radiation than is recommended. The studies point out the need for patients and their doctors to discuss any test that is ordered to diagnose illness or injury. The doctor should explain why a test is needed, what questions the test is going to help answer and why a particular test is the best choice.
One can conclude that exposure to a CT scan increases the risk of getting cancer by 2%
References:
American College of Radiology and Radiological Society of North America (April 2012). Patient Safety: Radiation Dose in X-Ray and CT ExamsExit Disclaimer. Retrieved July 19, 2013.
U.S. Food and Drug Administration (August 2009). What are the Radiation Risks from CT? Retrieved July 19, 2013.
Howlader N, Noone AM, Krapcho M, et al. (eds). SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, 2013 (http://seer.cancer.gov/csr/1975_2010/).
Berrington de González A, Mahesh M, Kim K-P, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Archives of Internal Medicine 2009; 169(22):2071–2077. [PubMed Abstract]
Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Archives of Internal Medicine 2009; 169(22):2078–2086. [PubMed Abstract]
Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII—Phase 2. Washington, DC: The National Academies Press, 2006.
Frush DP, Donnelly LF, Rosen NS. Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 2003; 112(4):951–957. [PubMed Abstract]
Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380(9840):499–505. [PubMed Abstract]
Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. British Medical Journal 2013 May 21; 346:f2360. doi:10.1136/bmj.f2360Exit Disclaimer
Neumann RD, Bluemke DA. Tracking radiation exposure from diagnostic imaging devices at the NIH. Journal of the American College of Radiology 2010; 7(2):87–89. [PubMed Abstract]