HOPEFUL STEPS TOWARD A RAPID SALIVA-BASED TEST FOR COVID-19 ANTIBODIES
by
Danny Jacobs and Robert Gorter, MD, PhD.
March 10th 2021
A research collaboration born in the lab of Johns Hopkins microbiologist Christopher Heaney aims to scale up rapid testing to track spread of the virus
When COVID-19 cases started ticking up across the U.S. a year ago, Christopher Heaney and his research team at the Johns Hopkins Bloomberg School of Public Health went into high gear, supporting several research studies with their lab’s saliva collection and antibody testing expertise. These included investigations testing for antibodies for SARS-CoV-2, the virus that causes COVID-19, using a simple saliva test that is less invasive than standard blood tests. Back in their lab, Heaney and his team processed the tests, and researchers have used the results to track the spread of the virus, including among people who never exhibited symptoms.
Saliva tests are Heaney’s specialty. He and his team used them to survey workers at industrial livestock operations in eastern Northern Carolina for hepatitis E, which in the U.S. is commonly transmitted to humans from swine. Heaney has used saliva tests to track hepatitis E in Bangladesh and norovirus infections in Peru. His lab has also refined saliva tests to detect exposure to and infection with antimicrobial-resistant bacteria such as Staphylococcus aureus and influenza viruses.

Chris Heaney
“With each new pathogen we’ve taken on, this salivary antibody measurement approach has brought a new perspective about how to contribute to the scientific body of knowledge concerning exposure and infection,” says Chris Heaney, who heads the Environmental Health Microbiology and Immunology Laboratory.
Heaney has been seeking opportunities to transition his lab’s test, which has to be performed in a centralized lab, to a rapid testing point-of-care platform. Such a rapid test could help improve understanding of the dynamic changes in the transmission of COVID-19 over time at population scale. The rapid test’s development will be accelerated thanks to a sponsored research agreement with GBS Inc., a life sciences company that is developing real-time point-of-care tests for COVID-19 and diabetes.
“We are privileged to collaborate with Dr. Heaney and his team at the Johns Hopkins Bloomberg School of Public Health to advance their world-leading research, and to contribute to Dr. Heaney’s mission to develop ‘last mile’ diagnostic options for patients globally,” says GBS Inc. CEO Harry Simeonidis.
The research agreement was facilitated by Johns Hopkins Technology Ventures. Patrick Ho, director of Life Science Technology Development at JHTV, has been working with Heaney since he disclosed his technology, helping attract funding and advising on business decisions in an effort to commercialize Heaney’s work as quickly as possible.
“It’s been an ideal interaction,” Ho says. “The synergy between the reliance on my team for business advice and my reliance on him for the science and his knowledge, it just clicked.”
To scale up the saliva antibodies test, Heaney is seeking emergency use authorization for the technology from the U.S. Food and Drug Administration, which allows unapproved medical products to be used to diagnose life-threatening diseases when there are no approved alternatives.
Saliva samples can be collected at home or in remote locations. They can also be gathered more frequently and quickly, particularly among large or disproportionately impacted groups.
“Once we knew that there are enough antibodies in saliva from adults to diagnose a prior infection, we also wanted to see if the test could work in children,” says Nora Pisanic, an assistant scientist in Heaney’s lab. In one ongoing study, Pisanic and colleagues asked participants to help their smaller children and infants give a saliva sample and found the test can be used across all ages to see whether somebody has been infected previously.
“How can we bring rigor to community-based studies of infectious disease dynamics without creating a burden? That’s where saliva comes in,” says Heaney, an associate professor in the Department of Environmental Health and Engineering. “Everything about SARS-CoV-2’s impact is uncovering structural inequities, where the barriers and lack of access to testing are most pronounced.”

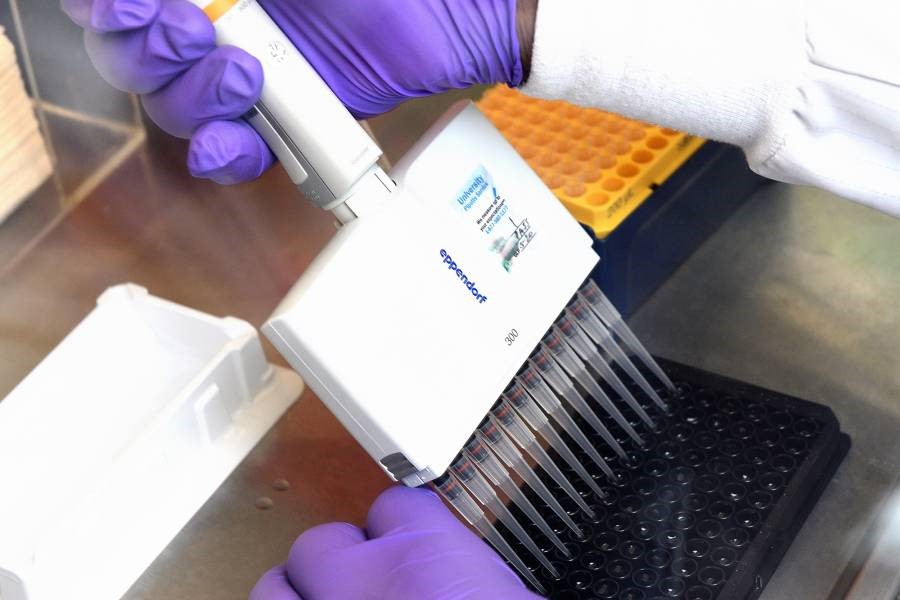
Nora Pisanic, an assistant scientist in Heaney’s lab, loads samples into a test device in the lab (WILL KIRK / JOHNS HOPKINS UNIVERSITY)
The scaled-up antibody test results will also help researchers and decision-makers understand dynamic changes in COVID-19, including the pace of trajectories toward herd immunity versus immunity gaps. The latter could be used to help prioritize use of vaccines.
In addition to Heaney’s team’s early SARS-CoV-2 antibody testing, many of his colleagues at the School of Public Health added a saliva protocol to their research after he shared early data showing saliva’s equivalence to blood-based antibody tests and its diagnostic accuracy to identify COVID-19 cases. (A paper documenting the data was published in December.)
Ultimately, Heaney would like to convert his lab into a center or institute focused on community science and innovation for environmental justice, where saliva-based and other tests, like the one for the coronavirus, are applied equitably and distributed to places where they are needed the most.
“That’s our core goal,” he says. “Our reason to keep innovating as a lab is to address the unmet scientific needs of the most disproportionately impacted communities.”
Dr. Gorter: let me explain the difference between qualitative testing and quantitative testing…….
Qualitative testing
A qualitative test is often the first port of call in general COVID-19 testing, and the most traditional type of testing used in infectious disease. By detecting SARS-CoV-2 antibodies in a blood sample, this diagnostic assay provides a simple “yes or no” answer as to whether or not antibodies are present. However, qualitative testing cannot measure how many SARS-CoV-2 antibodies are present, and it doesn’t indicate the strength of the immune response. In some cases, just knowing that a patient has developed an immune response to the virus is all the clinical information that’s needed.
Quantitative and semi-quantitative testing
A qualitative test determines the “if;” quantitative and semi-quantitative tests answer the question “how much?” By measuring the level of SARS-CoV-2 antibodies in a patient’s blood sample, quantitative and semi-quantitative tests give a more definitive answer about the body’s immune response to the virus. Quantitative tests are traceable to a specific international standard (recently set by he WHO) that ensures the result produced correlates to a numeric quantity of antibodies. Due to the current lack of an international standard, the FDA has not granted EUA to any quantitative tests. Semi-quantitative tests estimate an approximate concentration of SARS-CoV-2 antibodies in a patient’s blood sample, and can be measured against a specific standard to ensure consistent results. These tests are now being deployed if a patient has already received a positive qualitative result, or if the doctor suspects a patient has previously been infected with COVID-19 by determination of an antigen test and /or the clinical picture.
Quantitative and semi-quantitative tests are poised to play a vital role in the development of COVID-19 vaccines that aim to trigger a pre-emptive antibody response. By measuring the body’s immune response over time, scientists can use these tests to determine which vaccines are most effective and how long that effectiveness will last.
Additionally, quantitative and semi-quantitative testing can help guide the allocation of plasma donations from recovered COVID-19 patients to current patients by identifying which donors have the highest level of antibodies. Plasma from those donors is likely to offer the greatest benefit to patients who are currently sick.
Because so much is still unknown about the behavior of this novel coronavirus, it’s important to note that the basic presence of SARS-CoV-2 antibodies is not currently a reliable indicator of immunity to repeat or future infections. One should determine the amount of antibodies and of they are above a minimum value, the person is immune.
In Germany, for instance, the Rudolf Koch Institute (RKI) has determined that if someone has high levels of antibodies (as directed by the WHO), that person does not need to be injected with the current mRNA injections.