Ionizing air affects influenza virus infectivity and prevents airborne-transmission
Hagbom M, Nordgren J, Nybom R, Hedlund KO, Wigzell H, Svensson L. Ionizing air affects influenza virus infectivity and prevents airborne-transmission in: Sci Rep. 2015;5:11431. Published 2015 Jun 23. doi:10.1038/srep11431
January 10th, 2021
Bipolar ionization is experiencing a recent surge in popularity as the coronavirus pandemic triggers concerns about air quality.
Integrated into ventilation and air-conditioning systems, the technology utilizes specialized tubes that take oxygen molecules from the air and convert them into charged atoms that then cluster around micro-particles, surrounding and deactivating harmful substances like airborne mold, bacteria, allergens, and viruses.
They also attach to expelled breath droplets and dust particles that can transport viruses, enlarging them so they’re more easily caught in filters. It is an active process that provides continuous and complete disinfection.
“The ions produce a chemical reaction on the cell membrane surface that inactivates the virus,” Philip Tierno, clinical professor of microbiology and pathology at the NYU School of Medicine. “It can reduce 99.9% of all microbes in a matter of minutes.”
This equipment is not expensive and one can even buy very effective pocket-size devices which run on routine rechargeable 12 Volt batteries
Even published by the NIH, there are literally hundreds of peer-reviewed studies showing the huge benefits of ionization of the air in rooms, nursing homes and hospitals, etc.
Many large venues already employ bipolar ionization: hospitals including Johns Hopkins, Children’s Hospital Boston and the University of Maryland Medical Center have already embraced the technology.
Bipolar ionization has been used in healthcare for many years for many applications. Dr. Gorter: I believe bipolar ion systems will become a standard in these critical environments to protect patients and staff in the USA and the EU.
In the US, terminals at LaGuardia, O’Hare, LAX, and San Francisco International Airports already have ionizing air units in place. Tampa’s Amalie Arena and the TWA Hotel at JFK airport are adopting bipolar ionization technology, as are large workplaces such as Google’s headquarters in Chicago and San Jose.
There are also options for the home, including standalone portable devices and additions to HVAC systems.
Recently, in The Netherlands, the representatives of both the Eerste Kamer (Upper House, Senate) with 75 members and the Tweede Kamer (Lower House, Congress, Bundestag) with 150 members (and public galleries) installed in their meeting halls bipolar ionization equipment to kill 99,9% of ALL possible viruses; including all Corona viruses.
Unfortunately, this was a well-kept secret and the cabinet refused to install this equipment in hospitals, nursing homes or at airports. It has been a conscious decision to go for lockdowns and universal vaccinations instead.
Abstract
By the use of a modified ionizer device we describe effective prevention of airborne transmitted influenza A (strain Panama 99) virus infection between animals and inactivation of virus (>97%). Active ionizer prevented 100% (4/4) of guinea pigs from infection. Moreover, the device effectively captured airborne transmitted calicivirus, rotavirus and influenza virus, with recovery rates up to 21% after 40 min in a 19 m3 room. The ionizer generates negative ions, rendering airborne particles/aerosol droplets negatively charged and electrostatically attracts them to a positively charged collector plate. Trapped viruses are then identified by reverse transcription quantitative real-time PCR. The device enables unique possibilities for rapid and simple removal of virus from air and offers possibilities to simultaneously identify and prevent airborne transmission of viruses.
There is an urgent need for simple, portable and sensitive devices to collect, eliminate and identify viruses from air, to rapidly detect and prevent outbreaks and spread of infectious diseases. Each year, infectious diseases cause millions of deaths around the world and many of the most common infectious pathogens are spread by droplets or aerosols caused by cough, sneeze, vomiting etc.2,3,4,5. Knowledge of aerosol transmission mechanisms are limited for most pathogens, although spread by air is an important transmission route for many pathogens including viruses6.
Today, no simple validated technology exists which can rapidly and easily collect viruses from air and identify them. The problem is not the analyzing technique, since molecular biological methods such as real-time PCR enable a sensitive detection system of most pathogens. The difficulty is to develop an effective sampling method to rapidly collect small airborne particles including viruses from large volumes of air. Furthermore, the sampling method should be robust with easy handling to enable a wide distribution and application in many types of environment. At present, the most commonly used techniques aimed to collect pathogens from air are airflow and liquid models. These systems are complex, and their efficiency has not been thoroughly evaluated.
Spread of infectious diseases in hospitals can be most significant. In many situations, there is a need for a pathogen- and particle-free environment, e.g. in operation wards, environments for immunosuppressed patients as well as for patients with serious allergies. This makes it desirable to have a method not only for collection and identification, but also for eliminating virus and other pathogens from air. Ozone gas has been shown to inactivate norovirus and may be used in empty rooms to decontaminate surfaces, however in rooms with patients ozone should not been used due to its toxicity. Generation of negative ions has previously been shown to reduce transmission of Newcastle disease virus and several kind of bacteria in animal experimental set-ups.
The ionizing device used in this study operates at 12 V and generates negative ionizations in an electric field, which collide with and charge the aerosol particles. Those are then captured by a positively charged collector plate. For safety reasons, the collector plate has a very low current, less than 80μA, however the ionizer accelerates a voltage of more than 200,000 eV, which enables high production of several billion electrons per second. Moreover, this device does not produce detectable levels of ozone and can thus be safely used in all environments.
This technique of ionization of the air is known to effectively collect and eliminate cat-allergens from air. Aerosolized rotavirus, calicivirus and influenza virus particles exposed to the ionizing device were attracted to the collector plate and subsequently identified by electron microscopy and reverse transcription quantitative real-time PCR techniques. Most importantly, we demonstrate that this technology can be used to prevent airborne-transmitted influenza virus infections effectively in any space; including hospitals and home for the elderly.
Results
Visualization and efficiency of aerosol sampling were determined by electron microscopy
To develop and validate the ionizing technique for collection and identification of viral pathogens, we used several viruses of clinical importance; calicivirus, rotavirus and influenza virus (H3N2, strain Salomon Island) as well as latex particles. Canine calicivirus (CaCV, strain 48) was used as a surrogate for human norovirus, the etiological agent behind the “winter vomiting disease”, causing outbreaks of great clinical and economic importance. Rhesus rotavirus was used as a surrogate marker for human rotavirus.
The device (Fig. 1) consists of a small portable 12 volt operated ionizer, with a collector plate of positive charge attached to the ionizer, attracting negative particles from the air by electrostatic attraction. To determine optimal time collection parameters, latex particles with sizes ranging from <1 to >10 μm were nebulized into a room of 19 m3. Testing revealed that 40–60 min was required to eliminate >90% of free latex particles in the air as determined by real-time particle counting (PortaCount Plus). The particle counter can detect particles with size greater than 0.02 μM. Visualization by scanning electron microscopy (SEM) on grids from active- and inactive ionizer collector plates showed that accumulation of latex particles was dramatically enhanced on active ionizer collector plates compared to the inactive (Fig. 1). Next, high numbers of rotavirus and formalin-inactivated influenza virus were aerosolized under the same conditions. While, after 40 min the inactive collector plates contained few (<5) rotavirus and influenza virus, the active collector contained >50 virus particles, as determined by transmission electron microscopy (TEM), (Fig. 1).
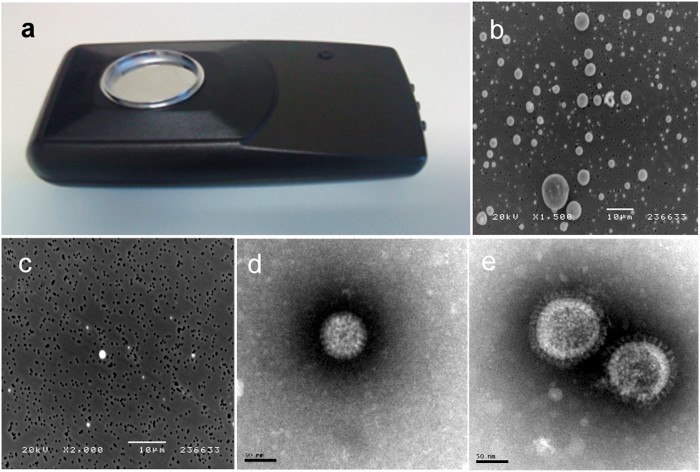
Figure 1: Airpoint ionizer with collector plate (size 13 × 35 cm) (a). The ionizing device was developed based of the Ion-Flow Ionizing Technology from LightAir AB, Solna, Sweden and was modified by installing a plastic-cup with a conductive surface of 47 mm in diameter, with positive charge, as the collector plate; Aerosolized and trapped latex particles (>1 to <10 μm) on active (b) and inactive (c) ionizer, (bar = 10 μM); Rotavirus (d); and influenza virus (H1N1; strain Salomon Island) (e) trapped on active ionizer, (Bar = 50 nm).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4477231/
https://pubmed.ncbi.nlm.nih.gov/7702504/
https://www.cambridge.org/…air-ionization-on…airborne…virus…/ 9C512E33141BB29482702596DBF993F9/
https://fsg.com/bipolar-ionization-inactivate-pathogens-viruses-facilities/
https://www.businessinsider.com/bipolar-ionization-could-be-a-secret-weapon -against-covid-19-2020-4
References
Lipsitch M. et al. Transmission dynamics and control of severe acute respiratory syndrome. Science 300, 1966–1970, (2003). [PMC free article] [PubMed] [Google Scholar]
Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface 6 Suppl 6, S783–S790, (2009). [PMC free article] [PubMed] [Google Scholar]
Stilianakis N. I. & Drossinos Y. Dynamics of infectious disease transmission by inhalable respiratory droplets. J R Soc Interface 7, 1355–1366, (2010). [PMC free article] [PubMed] [Google Scholar]
Teunis P. F., Brienen N. & Kretzschmar M. E. High infectivity and pathogenicity of influenza A virus via aerosol and droplet transmission. Epidemics 2, 215–222, (2010). [PubMed] [Google Scholar]
Fowler R. A., Scales D. C. & Ilan R. Evidence of airborne transmission of SARS. N Engl J Med 351, 609–611; author reply 609-611, (2004). [PubMed] [Google Scholar]
Fiegel J., Clarke R. & Edwards D. A. Airborne infectious disease and the suppression of pulmonary bioaerosols. Drug Discov Today 11, 51–57, (2006). [PMC free article] [PubMed] [Google Scholar]
Nordgren J., Bucardo F., Svensson L. & Lindgren P. E. Novel light-upon-extension real-time PCR assay for simultaneous detection, quantification, and genogrouping of group A rotavirus. J Clin Microbiol 48, 1859–1865, (2010). [PMC free article] [PubMed] [Google Scholar]
Nordgren J., Bucardo F., Dienus O., Svensson L. & Lindgren P. E. Novel light-upon-extension real-time PCR assays for detection and quantification of genogroup I and II noroviruses in clinical specimens. J Clin Microbiol 46, 164–170, (2008). [PMC free article] [PubMed] [Google Scholar]
Mackay I. M., Arden K. E. & Nitsche A. Real-time PCR in virology. Nucleic Acids Res 30, 1292–1305, (2002). [PMC free article] [PubMed] [Google Scholar]
Booth T. F. et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis 191, 1472–1477, (2005). [PMC free article] [PubMed] [Google Scholar]
Hermann J. R. et al. Optimization of a sampling system for recovery and detection of airborne porcine reproductive and respiratory syndrome virus and swine influenza virus. Appl Environ Microbiol 72, 4811–4818, (2006). [PMC free article] [PubMed] [Google Scholar]
Pyankov O. V. et al. Using a bioaerosol personal sampler in combination with real-time PCR analysis for rapid detection of airborne viruses. Environ Microbiol 9, 992–1000, (2007). [PubMed] [Google Scholar]
Verreault D., Moineau S. & Duchaine C. Methods for sampling of airborne viruses. Microbiol Mol Biol Rev 72, 413–444, (2008). [PMC free article] [PubMed] [Google Scholar]
Turgeon N., Toulouse M. J., Martel B., Moineau S. & Duchaine C. Comparison of five bacteriophages as models for viral aerosol studies. Appl Environ Microbiol 80, 4242–4250, (2014). [PMC free article] [PubMed] [Google Scholar]
Verani M., Bigazzi R. & Carducci A. Viral contamination of aerosol and surfaces through toilet use in health care and other settings. American journal of infection control 42, 758–762, (2014). [PMC free article] [PubMed] [Google Scholar]
Brankston G., Gitterman L., Hirji Z., Lemieux C. & Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis 7, 257–265, (2007). [PubMed] [Google Scholar]
Sato T. [Infection control in hospitals]. Masui 59, 56–63, (2010). [PubMed] [Google Scholar]
Hans C. Infection control practices for avian influenza in healthcare facilities. J Indian Med Assoc 104, 388, 390, 392 passim, (2006). [PubMed] [Google Scholar]
Hatagishi E. et al. Establishment and clinical applications of a portable system for capturing influenza viruses released through coughing. PloS one 9, e103560, (2014). [PMC free article] [PubMed] [Google Scholar]
Bergeron V. et al. Supplemental treatment of air in airborne infection isolation rooms using high-throughput in-room air decontamination units. American journal of infection control 39, 314–320, (2011). [PubMed] [Google Scholar]
Hudson J. B., Sharma M. & Petric M. Inactivation of Norovirus by ozone gas in conditions relevant to healthcare. The Journal of hospital infection 66, 40–45, (2007). [PubMed] [Google Scholar]
Mitchell B. W. & King D. J. Effect of negative air ionization on airborne transmission of Newcastle disease virus. Avian diseases 38, 725–732, (1994). [PubMed] [Google Scholar]
Estola T., Makela P. & Hovi T. The effect of air ionization on the air-borne transmission of experimental Newcastle disease virus infections in chickens. The Journal of hygiene 83, 59–67, (1979). [PMC free article] [PubMed] [Google Scholar]
Escombe A. R. et al. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS medicine 6, e43, (2009). [PMC free article] [PubMed] [Google Scholar]
Gast R. K., Mitchell B. W. & Holt P. S. Application of negative air ionization for reducing experimental airborne transmission of Salmonella enteritidis to chicks. Poultry science 78, 57–61, (1999). [PubMed] [Google Scholar]
Parvaneh S. et al. A new method for collecting airborne allergens. Allergy 55, 1148–1154, (2000). [PubMed] [Google Scholar]
Mochizuki M. et al. A calicivirus isolated from a dog with fatal diarrhoea. Vet Rec 132, 221–222, (1993). [PubMed] [Google Scholar]
Lee B. Y. et al. Economic value of norovirus outbreak control measures in healthcare settings. Clinical microbiology and infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases 17, 640–646, (2011). [PMC free article] [PubMed] [Google Scholar]
Vesikari T., Rautanen T., Varis T., Beards G. M. & Kapikian A. Z. Rhesus Rotavirus candidate vaccine. Clinical trial in children vaccinated between 2 and 5 months of age. Am J Dis Child 144, 285–289, (1990). [PubMed] [Google Scholar]
Istrate C. et al. Bone marrow dendritic cells internalize live RF-81 bovine rotavirus and rotavirus-like particles (RF 2/6-GFP-VLP and RF 8*2/6/7-VLP) but are only activated by live bovine rotavirus. Scand J Immunol 65, 494–502, (2007). [PubMed] [Google Scholar]
Lowen A. C., Mubareka S., Tumpey T. M., Garcia-Sastre A. & Palese P. The guinea pig as a transmission model for human influenza viruses. Proc Natl Acad Sci U S A 103, 9988–9992, (2006). [PMC free article] [PubMed] [Google Scholar]
Pica N., Chou Y. Y., Bouvier N. M. & Palese P. Transmission of influenza B viruses in the guinea pig. J Virol 86, 4279–4287, (2012). [PMC free article] [PubMed] [Google Scholar]
Mubareka S. et al. Transmission of influenza virus via aerosols and fomites in the guinea pig model. J Infect Dis 199, 858–865, (2009). [PMC free article] [PubMed] [Google Scholar]
Gralton J., Tovey E., McLaws M. L. & Rawlinson W. D. The role of particle size in aerosolised pathogen transmission: a review. J Infect 62, 1–13, (2011). [PMC free article] [PubMed] [Google Scholar]
Kettleson E. M. et al. Airborne virus capture and inactivation by an electrostatic particle collector. Environ Sci Technol 43, 5940–5946, (2009). [PubMed] [Google Scholar]
Murray B. K. et al. Virion disruption by ozone-mediated reactive oxygen species. Journal of virological methods 153, 74–77, (2008). [PubMed] [Google Scholar]
Nishikawa K. & Nojima H. Airborn virus inactivation technology using cluster ions generated by discharge plasma. Sharp Tech J 86, 10–15, (2003). [Google Scholar]
Lowen A. C., Mubareka S., Steel J. & Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 3, 1470–1476, (2007). [PMC free article] [PubMed] [Google Scholar]
Lowen A. C., Steel J., Mubareka S. & Palese P. High temperature (30 degrees C) blocks aerosol but not contact transmission of influenza virus. J Virol 82, 5650–5652, (2008). [PMC free article] [PubMed] [Google Scholar]
Lowen A. C. et al. Blocking interhost transmission of influenza virus by vaccination in the guinea pig model. J Virol 83, 2803–2818, (2009). [PMC free article] [PubMed] [Google Scholar]
Andersson J. et al. Rapid detection of cytomegalovirus using immune scanning electron microscopy. Journal of virological methods 16, 253–262, (1987). [PubMed] [Google Scholar]
Wetterberg L. et al. Micrometer-sized particles in cerebrospinal fluid (CSF) in patients with schizophrenia. Neurosci Lett 329, 91–95, (2002). [PubMed] [Google Scholar]
Johansson V. et al. Microscopic particles in two fractions of fresh cerebrospinal fluid in twins with schizophrenia or bipolar disorder and in healthy controls. PloS one 7, e45994, (2012). [PMC free article] [PubMed] [Google Scholar]
Nordgren J., Kindberg E., Lindgren P. E., Matussek A. & Svensson L. Norovirus gastroenteritis outbreak with a secretor-independent susceptibility pattern, Sweden. Emerging infectious diseases 16, 81–87, (2010). [PMC free article] [PubMed] [Google Scholar]
San Gabriel M. C. et al. Identification of canine calicivirus capsid protein and its immunoreactivity in western blotting. The Journal of veterinary medical science / the Japanese Society of Veterinary Science 59, 97–101, (1997). [PubMed] [Google Scholar]
Nilsson A. C. et al. Longitudinal clearance of seasonal influenza A viral RNA measured by real-time polymerase chain reaction in patients identified at a hospital emergency department. Scandinavian journal of infectious diseases 42, 679–686, (2010). [PubMed] [Google Scholar]